For decades, medical research has relied heavily on statistical
correlations to identify potential risk factors for diseases.
Observational studies linking smoking to lung cancer or cholesterol to
heart disease have undoubtedly saved millions of lives. However, as we
venture into the era of precision medicine, the limitations of
correlation-based approaches are becoming increasingly apparent. The
emergence of causal inference engines promises to revolutionize how we
understand disease etiology by distinguishing true causation from mere
association.
The fundamental challenge in medical research lies in the fact that
correlation does not imply causation. Traditional epidemiological
methods often struggle to account for confounding variables - hidden
factors that influence both the presumed cause and the observed
effect. This has led to numerous instances where initially promising
associations failed to hold up under more rigorous scrutiny. The
famous example of hormone replacement therapy (HRT) and cardiovascular
disease serves as a cautionary tale; early observational studies
suggested a protective effect, while later randomized controlled
trials revealed increased risks.
Causal inference engines represent a paradigm shift in analytical
methodology.
These sophisticated computational frameworks combine principles from
statistics, computer science, and epidemiology to reconstruct the
underlying causal structures from complex datasets. Unlike traditional
methods that simply measure associations, causal models attempt to
answer "what if" questions by simulating interventions. This approach
is particularly valuable in situations where randomized controlled
trials are impractical or unethical, such as studying the long-term
effects of environmental exposures or lifestyle factors.
At the heart of these engines lie directed acyclic graphs (DAGs) and
counterfactual reasoning. DAGs provide visual representations of
assumed causal relationships, helping researchers explicitly state
their hypotheses about how variables influence each other.
Counterfactual analysis, on the other hand, asks how outcomes would
differ if a particular factor were changed while holding everything
else constant. Together, these tools enable researchers to move beyond
surface-level patterns and probe deeper into the mechanisms driving
disease development.
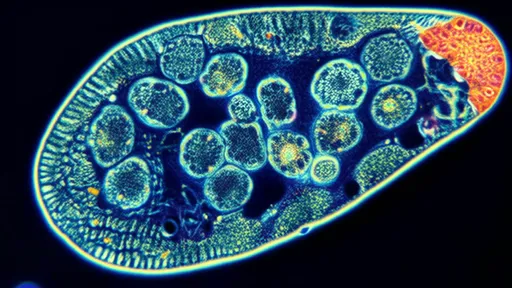
The application of causal inference in genomic medicine offers
particularly exciting possibilities. Genome-wide association studies
(GWAS) have identified thousands of genetic variants correlated with
various diseases, but determining which variants actually contribute
to disease pathogenesis remains challenging. Causal inference methods
can help prioritize variants for functional studies by estimating
their likely causal effects, potentially accelerating the translation
of genetic discoveries into clinical applications.
Real-world evidence (RWE) represents another area where causal
inference engines are making significant impacts.
As healthcare systems increasingly digitize patient records,
researchers gain access to vast troves of observational data. However,
analyzing this data without proper causal frameworks risks drawing
erroneous conclusions. Advanced methods like propensity score
matching, instrumental variable analysis, and doubly robust estimation
are enabling researchers to extract more reliable insights from these
complex, messy datasets.
Despite their promise, causal inference engines are not without
limitations. The quality of their output depends heavily on the
validity of the underlying assumptions, which are often unverifiable
from the data alone. Moreover, these methods typically require larger
sample sizes than conventional analyses and can be computationally
intensive. There's also an ongoing need to educate the medical
research community about proper implementation and interpretation of
these techniques to prevent misuse.
Looking ahead, the integration of causal inference with artificial
intelligence and machine learning presents fascinating opportunities.
While AI excels at pattern recognition, it often struggles with causal
reasoning. Combining these approaches could yield systems capable of
not only identifying associations but also suggesting plausible causal
mechanisms and generating testable hypotheses. Such systems might
eventually help clinicians predict how individual patients will
respond to specific treatments, moving us closer to the promise of
truly personalized medicine.
The ethical implications of causal inference in healthcare deserve
careful consideration. As these methods become more sophisticated,
they may reveal uncomfortable truths about disease causation that
challenge existing paradigms or implicate powerful industries. The
tobacco industry's decades-long resistance to accepting smoking's
causal role in lung cancer serves as a sobering reminder of how
economic interests can conflict with scientific evidence. Robust
safeguards will be needed to ensure that causal findings translate
into public health action when warranted.
In clinical practice, causal inference could transform diagnostic
processes and treatment decisions.
Rather than relying on population-level statistics that may not apply
to individual patients, physicians could use causal models to assess
how specific factors contribute to a particular patient's condition.
This approach might be especially valuable for complex, multifactorial
diseases like diabetes or autoimmune disorders, where numerous genetic
and environmental influences interact in poorly understood ways.
The development of user-friendly causal inference tools is helping
democratize these methods beyond academic biostatistics departments.
New software platforms allow researchers with modest technical
backgrounds to apply sophisticated causal techniques to their data.
However, experts caution against viewing these tools as black boxes -
meaningful causal analysis still requires deep subject-matter
knowledge and careful consideration of potential biases.
As the field progresses, we're likely to see causal inference engines
incorporated into routine public health surveillance systems. This
could enable earlier detection of emerging health threats and more
accurate assessment of intervention effectiveness. During the COVID-19
pandemic, for instance, causal methods helped disentangle the effects
of various mitigation strategies from confounding factors like
seasonality and population mobility patterns.
The journey from correlation to causation in medicine has been long
and fraught with missteps. While causal inference engines don't offer
a perfect solution, they represent our best hope for building a more
accurate understanding of disease causation. As these methods continue
to evolve and mature, they may finally allow us to move beyond the
limitations of correlation-based thinking and develop more effective
strategies for disease prevention and treatment.